What Does the Vagus Nerve Have to Do With Testosterone?
- By Rebekah Harding
- November 6, 2023
30-Second Takeaway
- Up to 29 percent of deployed soldiers who served in OEF or OIF developed PTSD.
- People with PTSD may blunted cortisol responses to stress, which may give way to symptoms like depression, anxiety, poor immune function, and brain fog.
- Flattened cortisol levels can increase inflammation, which may contribute to low testosterone.
- Functional medicine doctors believe that vagus nerve stimulation can improve cortisol response in veterans with PTSD.
C
ombat changes you forever. Ask any veteran and that’s what they’ll tell you. The reason? Functional medicine experts suspect that the relationship between your vagus nerve, stress response, and testosterone could be part of the equation.
Post-traumatic stress disorder (PTSD) disproportionately affects military personnel. The National Center for PTSD estimates that 7 out of 100 veterans will develop the condition, which is characterized by flashbacks, nightmares, and severe anxiety after a person goes through a traumatic event. For more specific campaigns—like Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF)—up to 29 percent of deployed soldiers have developed PTSD. To put it into perspective, only 6 percent of the non-military adult population will experience PTSD at some point in their lives.
The impact of PTSD on post-deployment quality of life goes far deeper than the debilitating mental and emotional symptoms. What functional medicine doctor Anastasia Jandes, M.D., began to notice after working with veterans through the VA: many vets with PTSD also had low testosterone.
“Field training drops testosterone by almost 50 percent,” Jandes tells Hone Health CEO Saad Alam on a recent episode of the Hone In podcast, referencing a 2020 study (1). “The scenarios that soldiers go through begins to create this fight or flight mode that stays entrained within the body. That stops the body’s natural state of rest and digest.”
Why does this happen? Jandes believes that the relationship between cortisol regulation and testosterone could be to blame. But the vagus nerve could hold the secret to better treatment and boosted healthspan.
How is chronic stress, inflammation, testosterone and veterans’ health connected? Dr. Jandes discusses how veterans can manage post-deployment hormone health concerns.
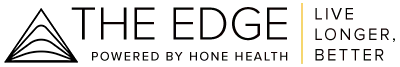
The Vagus Nerve and Cortisol
Picture the vagus nerve as a superhighway inside your body—spanning from your brain to your belly—that controls your heart rate, digestion, breathing, alertness, relaxation, and gut-brain connection.
When you’re in a stressful situation—like active combat—your sympathetic nervous system activates your adrenal glands, which produce cortisol (the stress hormone) to get you ready to jump into survival mode (2). Under normal circumstances, the vagus nerve helps to reel in the stress response and lower cortisol levels once the stressor is no longer present.
But exposure to active war zones makes it difficult for many soldiers to snap out of their stress response, even when they’re physically safe. This leads to adrenal burnout.
“If your adrenals become burnt out, you can’t really make cortisol. Your cortisol curve becomes flat, which means cortisol levels throughout the whole body start to go down,” Jandes explains. “Folks with PTSD have that.”
Research shows that some people with PTSD may have lower baseline cortisol levels or blunted cortisol responses to stress compared to individuals without PTSD (3). Low cortisol caused by adrenal burnout may give way to symptoms like depression, anxiety, poor immune function, brain fog, and loss of resilience in stressful situations—which can exacerbate PTSD symptoms and post-deployment mental health issues.
Cortisol and Testosterone
For veterans with PTSD, flattened cortisol levels are just the beginning of a vicious cycle: low cortisol exacerbates depression and poor sleep, depression and poor sleep can increase inflammation, and inflammation can impact testosterone levels.
“When we hit the reset button at night, the brain begins to find its own anti-inflammatory mechanisms to heal the body. That’s where the GI tract does the majority of its work. That’s when we make a lot of our hormones including testosterone,” Jandes explains. “Having stress interrupts sleep. Having PTSD interrupts sleep. And so all of it leads to more inflammation.”
But the hormone hamster wheel from hell doesn’t end there. Common symptoms of low testosterone include increased irritability, depression, and anxiety—which just adds to the mental health dumpster fire many vets are already dealing with.
“Testosterone is a natural anti-inflammatory. It’s a natural anti-anxiety. And it’s a natural antidepressant,” Jandes explains. “So for men, in particular, that cortisol to testosterone situation is pretty dicey.”
Without medical or therapeutic intervention—like behavioral health support or testosterone replacement therapy (TRT)—your body doesn’t have the tools to snap out of this pattern.
What Is Vagus Nerve Stimulation?
Jandes suspects that taking it back to the beginning of the stress response cycle—by stimulating the vagus nerve—could jumpstart your body’s cortisol management into working order.
“It would be great if in the military there were some training exercises to create vagal tone improvements and being able to pull yourself out of fight or flight when you’re not actively in combat,” Jandes notes. “But those things are usually reserved for private functioning institutions.”
In-office vagus nerve stimulation (also dubbed vagal building or vagal relaxation) involves a physician implanting a small device to send small electrical signals to the nerve through your neck. Most devices send pulses in intervals of 30 seconds on, five minutes off. While the device is sending pulses, you may feel a slight tingling or uncomfortable buzzing sensation in your throat.
Vagus nerve stimulation is FDA approved for the treatment of long-lasting, hard-to-treat depression and epilepsy. Several combat veterans on Reddit have reported great improvement in their mental health treatment using vagus nerve stimulation.
How to stimulate the vagus nerve
Implanted vagus nerve stimulation devices—which can run you $10,000—aren’t the only option.
“Simple things like deep breathing from the belly where the diaphragm moves versus the chest can activate the vagal response and calm the body,” Jandes says.
Cold exposure, massages, exercise, and acupuncture may also stimulate the vagus nerve. At-home VNS devices, like Sensate, can be placed on the neck and activated to stimulate the vagus.
References
1. Mantua, et al (2020). Sleep Loss During Military Training Reduces Testosterone in U.S. Army Rangers: A Two-Study Series.
2. Chu, et al (2022). Physiology, Stress Reaction.
3. Meewisse, et al (2018). Cortisol and post-traumatic stress disorder in adults.